- Date:
This seminar featured speakers and panelists discussing the importance of including underrepresented populations in research, with tips and real examples of successful approaches and lessons learned. This event was co-sponsored by the CTSI Participant Recruitment Program and School of Medicine Differences Matter Research Action Group.
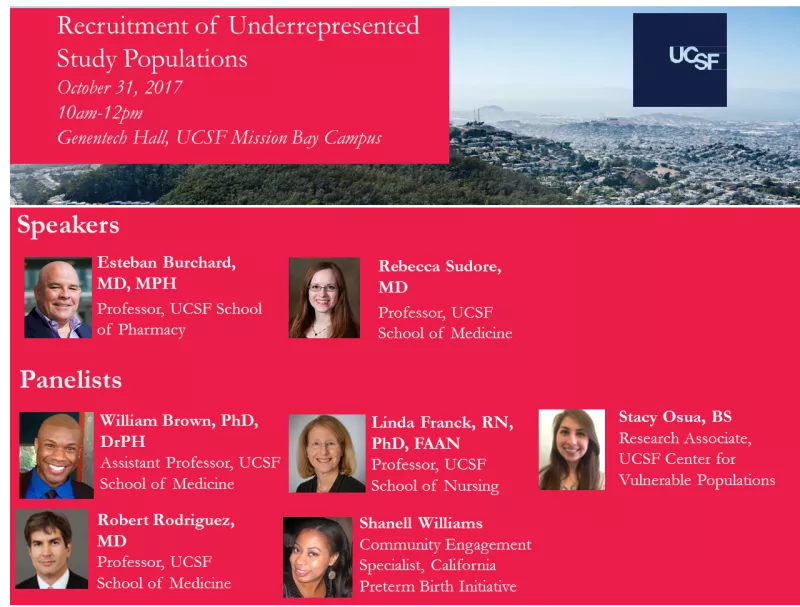
Speakers
Esteban Burchard, MD, MPH Professor, UCSF School of Pharmacy
Rebecca Sudore, MD Professor, UCSF School of Medicine
Panelists
William Brown, III, PhD, DrPH, Assistant Professor, UCSF School of Medicine
Linda Franck, RN, PhD, FAAN, Professor, UCSF School of Nursing
Stacy Osua, BS, Research Associate, UCSF Center for Vulnerable Populations
Robert Rodriguez, MD, Professor, UCSF School of Medicine
Shanell Williams, Community Engagement Specialist, California Preterm Birth Initiative
Q&A From Session
Community Advisory Board and participant engagement questions answered by Linda Franck, RN, PhD, FAAN and Shanell Williams:
What steps do you take to make sure your research teams and staff are trained to be culturally sensitive?
- There are excellent training resources at UCSF and that is a great place to start. Cultural sensitivity is not a ‘one-and-done’ training issue and it require an ongoing commitment to making time on a regular basis to have ongoing dialog to continuously raise awareness and sensitivity.
- Research teams need to be mindful of diversity in team composition in terms of gender, race and socioeconomic background. Having individuals on the team that bring varied cultural understanding can assist in ongoing conversations and training about cultural sensitivity, basis and humility.
Several speakers talked about getting results back to the community. What are some creative ideas to do this - not everyone likes lectures/ talks!
- Ideally, you will have community partners in the work. They will have some great creative ways of getting messages out about the research results, and they can often be the spokespersons for the work. We have seen great success with using social media and interviews (video or in person). Incorporating a discussion about the study findings into community events such as health fairs is also a great way to get the word out about findings. Be sure to offer food and people will come.
- Engaging the individuals that participated in the study to develop a dissemination plan for their community is very effective. They understand the norms within their community and the ways individuals in their community want to receive information. We have seen a great response when we incorporate music, creative expression and healing into our dissemination activities.
What approach do you take when inviting new communities to participate in research studies?
- The first step is to find trusted community partners and to engage them in the recruitment process. Ideally, you engage them earlier, when the study is being designed – or even better, in authentically discovering what questions people in that community, with a particular condition, want to have researched.
What tips can you give us for establishing meaningful research partnerships with under-served communities?
- Invest in developing a long term relationship; learn about the issues of importance to that community and explore how you might work together to address those issues through partnership in research. Be attentive to keeping the relationship reciprocal – you are not there to ‘take’ their stories and issues and turn it into research. You must find a way for your relationship to add value to their work/lives even during the exploratory phase of the relationship.
- Value their time and experience with the condition or issue that is being researched. Keep in mind the historical trauma that under-served communities have experienced engaging in research and be aware that this may surface during your work together as well as resources for support.
How can a Community Advisory Board strengthen research recruitment efforts?
- Community Advisory Boards, or study advisory boards add great value to any research recruitment effort because individuals who have the condition being researched, or who live in communities affected by the condition, have tremendous wisdom to share about how their communities will receive the study, the study design, appropriate language for recruitment and consent materials and how to reach potential participants. If they become enthusiastic about the project, they can serve as effective ambassadors for recruitment. They are also an excellent resource for ideas when recruitment or retention issues arise.
What has been the most surprising thing you have learned about working with under-served communities to increase research engagement?
- When investment in long-term relationships are made (see tip above on establishing meaningful partnerships), it has been a wonderful surprise to see how engaged in research under-served communities can become – and how that adds incredible value to the research being done – in terms of enthusiastic recruitment and better quality results that are more likely to be implemented and improve outcomes.
- That under-served communities will make time to engage in research that they find meaningful, despite the many demands on their time and energy.
Participant-centered planning, staff training, and health literacy questions answered by Rebecca Sudore, MD and Stacy Osua, BS:
What steps do you take to make sure your research teams and staff are trained to be culturally sensitive?
HIRING: We did this in several ways. First, it is important to look to hire individuals with emotional intelligence and an interest or passion for the vulnerable group you may be working with. This can be found by observing their past work or volunteer experiences. For example, several of our CRC’s had volunteered at a free clinic or worked in some capacity with older adults. It is also important in the hiring process to present some scenarios that you think the applicant may encounter and hear how they may deal with the scenario.
STUDY MATERIAL DEVELOPMENT: For the study material, we also pilot tested all of our marketing and study materials with the target population. This included study scripts for recruitment, informed consent, etc. We cannot emphasize enough how important it is to have an advisory board that includes patients and the target population. It can be helpful to have all staff attend these meetings so they can hear directly from stakeholders what will work and what will not work.
TRAINING: Once these scripts were honed, we had our staff model these scripts and checklists in private YouTube videos on our research YouTube Channel. All staff were required to review these videos and to conduct role play exercises before they were observed for the first few interviews with participants. CRC’s had to be signed off on role play exercises before they could go on to live recruitment and interviewing. Furthermore, it is crucial to have weekly meetings where the team can discuss what is working, what is not working, what may be upsetting to participants, and how the materials may need to be updated or changed to meet the population’s needs. For individuals who were struggling with role playing exercises or in observed interviews, we would provide targeted feedback and repeat the role plays and observation until we felt individuals were properly trained.
How can you increase trust with potential participants when your recruitment methods are mostly over the phone?
We sent out opt-out post cards with our study branding information on it as well as the approved ZSFGH, VA, or UCSF logos to help foster trust. We also would periodically send out additional letters with the same logo and information. That way, when we called, many people already knew who we were. We also make sure to post fliers in the clinic as this also helped with recognition. In addition, we made sure to call from VA or ZSFG hospital phone lines so that the caller ID was a number they recognized. While speaking with them, if we had obtained permission to do so, we mentioned that we had received permission from their medical provider to tell them about the study. Furthermore, if patients still had trepidations, we offered to mail them additional information about the study, offered to meet them in clinic to tell them more about it, and provided any additional information that would be helpful for them to make an informed choice.
Working with older folks, you have to work with their families. How do you incorporate their families into the recruitment process?
Often times when we were calling for recruitment purposes or screening potential patient participants in clinic, we also spoke to their family members. For example, family members would often answer phone and ask for the reason we were calling or would have accompanied patients to their clinic appointment. During those instances, we would shared the same information about what our study is about and answer any questions the patient or their family or friends may have. Because family members were often the patients’ mode of transportation, we tried to work around the patient and the family/or friends schedule and offered to do appointments over the phone, at home, on clinic days, or other times that worked for both parties. If friends or family members wanted to accompany the participant to an in-person interview we made sure to have a comfortable waiting areas and snacks. We would also offer an approximate time the interviews would take so they could run errands and come pick up the patients after we were done. It is also important to note that we asked participants to provide the phone numbers of close family and friends who could help us follow-up with if for some reason they moved or their phone changed. This also helped to often make a connection with friends and family as well.
How can you accommodate participants’ schedules when your recruitment coordinators only work Monday-Friday from 9am-5pm?
We hired individuals with the expectation up front that the job would include an alternative schedule, nights or weekends. For individuals who were used to a 9-5 job, we asked our team to please consider the needs of our participants and consider helping to cover each other so we could ensure we had coverage most nights and weekends. Not all CRC’s were able to accommodate their schedule due to commitment outside of work, but we worked together as a team to ensure we met our study participants needs.
For example, we had full time staff who’s 40-hour work week included 1 or 2 weekend days. We also made sure to stagger schedules throughout the work day. For example, some staff would start at 8am, 10am, or noon so that we had ongoing coverage in the evenings.
We also adapted to a caseload work flow in which each full-time employee had a dedicated caseload. Each individual caseload manager was responsible for arranging their schedule to meet patient needs and/or coordinating with other team members to trade or schedule the participant during another team members’ work shift. For example, if a participant needed a Saturday appointment but the CRC only worked Monday –Friday, they would ask a weekend staff member to cover the Saturday interview (and vice versa).
How do you improve health literacy in recruitment materials?
Several members of our team, including the PI, are experts in health literacy, which is helpful. However, we always follow the criteria we listed in our CTSI talk which includes targeting the text to a 5th-grade reading level, using clear headings, white space, short sentences, and pictures or colors that may help describe the text.
- For more tips, see Interventions to Improve Care for Patients with Limited Health Literacy. Sudore RL, Schillinger D. J Clin Outcomes Manag. 2009 Jan 1;16(1):20-29.
- Measure reading difficulty at www.lexile.com
- The Suitability Assessment Method (SAM) rates text on 22 factors and 6 categories. The tool was published in Teaching Patients with Low Literacy Skills (Doak, Doak, & Root, 1996). This publication is now out of print but you can download the book at the previous link and view the SAM in Chapter 4, page 49.
